Abstract: Has the human rights movement helped entrench neoliberalism? Could it help displace it? This article analyzes “right to medicines” cases, arguing that human rights, even in “socioeconomic” form, can intensify inequality and reproduce neoliberal logics, where they are simply overlain upon the existing political economy. But other versions of human rights are possible too. By tracing the efforts of access to medicines groups to link the right to health to reforms of local and global intellectual property laws, I explore a form of human rights movement that has more transformative potential.
There is no more prominent language today for the demand for justice beyond borders than that of human rights. But is that language, and the movement associated with it, adequate to the challenges presented by our new Gilded Age? Over the past several decades, pervasive shifts in governance—privatization, financialization, deregulation, and the undermining of state systems of social protection and redistribution, for example—have produced deepening inequality and political and social crises around the world. Is it an accident that, as these ideas and policies ascended, human rights also took root around the world?
An influential group of critics has argued that the human rights movement in fact abetted this neoliberal advance. Naomi Klein, for example, maintains that one of the most formative campaigns of the modern human rights movement, the one against disappearances and torture in the Southern Cone of Latin America in the 1970s, “helped the Chicago School ideology to escape from its first bloody laboratory virtually unscathed.”1 In Argentina and Chile, terror was deliberately used to soften resistance to the introduction of radical free-market policies, she explains; and human rights activists failed, she contends, when they treated these acts as “abuses” instead of “tools that served clear political and economic ends.”2
Susan Marks broadens and updates Klein’s critique. While human rights organizations and experts have begun to address the root causes of the rights violations they decry, she asserts, they nonetheless typically fail to engage “the larger framework within which those conditions are systematically reproduced.”3 In this way, human rights have functioned “as a set of ‘blinders’ that narrow our field of vision and prevent us from seeing (and hence from challenging) the wider scene.”4 For example, even sophisticated work on the right to food, Marks urges, obscures the role of the global market order in creating a systemic basis for widespread hunger, malnutrition, and food crises.5 Hunger appears in the human rights idiom as a mistake, when it is instead the result of “planned misery.”6 Here, too, the argument is that human rights as a movement and discourse has limited our horizons, and deflected our attention from the deeper implications of the prevailing market order.
Sam Moyn offers a somewhat milder critique.7 The tragedy of human rights, he asserts, is that it demanded only a moral minimum of sufficient protection and resources, and had “nothing to say about material inequality.”8 The movement thus became a “powerless companion,” merely “nipping at the heels of the neoliberal giant whose path goes unaltered and unresisted.”9
As these accounts suggest, critics have primarily focused on human rights as it operates to shape discourse and thought. However, the human rights movement has also significantly influenced law around the world—as has neoliberalism. What would a close consideration of the legality of human rights, in a context particular enough to allow us to see how it might relate to the legality of neoliberalism, help us to see about their relation? Might human rights also have more radical potential if we consider aspects of the movement further from its mainstream?10
This paper addresses these questions via a consideration of the emerging “right to medicines” that has taken legal hold in a growing number of countries, supported by an access to medicines movement that has operated in loose relation to the established human rights movement.11 Each year in Brazil, tens of thousands of people “judicialize,” asking courts to order the government to provide them with one or more specific medicines. They almost always win.12 In Colombia, from 1999–2014, an estimated 1.3 million right-to-health cases were litigated, many targeting medicines, with patients prevailing about 80 per cent of the time.13 The trend is most prominent in these two countries, but not limited to them. Courts in Argentina, Costa Rica, Uruguay, India, and South Africa have also ordered governments to provide medicines to individuals to vindicate rights to health and life.14
For critics and defenders of human rights both, these cases are an important instance. They construct a serious, judicially enforceable right—a socioeconomic right—that has provided life-sustaining medicines to tens of thousands, even millions of people. If these cases succeed in some meaningful sense, it would be hard not to count them as evidence that human rights can be more progressive than critics have acknowledged, and even can help sustain and expand the kind of welfare state that is the predicate of a more fair and egalitarian order.15 But what, in fact, are their implications?
There is, today, sharp debate in human rights circles about precisely this question, mostly focused on the Brazilian and Colombian experiences. Critics like Octavio L. Motta Ferraz contend that right to medicines cases in Brazil “almost inevitabl[y]” undermine health equity because courts demand that medicines be provided regardless of their cost, but health budgets are necessarily limited.16 The lion’s share of the benefits of these cases, he sustains, will accrue to those who litigate—who are unlikely to be the very poorest. Similar arguments have been made about the Colombian cases.17 This critique echoes a broader one made by Daniel M. Brinks and Varun Gauri: social rights litigation in general, they contend, benefits those in the “middle of the social spectrum” because the poor have less access to courts.18
In response to this challenge, some scholars have sought to show that a substantial number of litigants in at least some regions are poor.19 But the concern about differential access to courts has been hard to dispel, and is compounded by evidence that litigants frequently obtain expensive and even ineffective medicines that are not recommended by or included in the national formularies that determine what public and private insurers must provide.20 If we incorporate both of these considerations, it seems plausible that the direct impact of this right, at least in Latin America, has been to accentuate rather than ameliorate health inequities.21
Litigation also has indirect effects. A newer body of scholarly literature argues that judicialization has triggered responses from other branches of government that have improved the healthcare system, particularly in Colombia,22 and perhaps more broadly facilitated legal empowerment and social mobilization.23 This may be. But what kind of change and mobilization have courts helped to facilitate? What logic is borne within these cases, and does it form the basis for more far-reaching, equitable change?
So far, the debate over judicialization has failed to engage a foundational aspect of the right to medicines cases: the political economy of medicines that they assume. These cases operate against a background of market ordering and private property rights that they typically neither see nor disturb. It is anchored by a World Trade Organization treaty that has helped reshape national law, particularly in the global South, requiring all members to adopt intellectual property laws similar to those prevailing in the North, and to offer patents on life-saving medicines. These patents—monopoly rights that are granted by states and enforced by courts—and not manufacturing costs are the overwhelming determinant of the budgetary implications of the right to medicines. The prevailing political economy in fact, as I will explain, structurally undermines equity, increasing prices without generating significant countervailing innovation to meet the needs of the global poor.
As Quinn Slobodian has described, neoliberalism mandates not the destruction of the state but the construction of a particular form of governance that protects capital from democratic demands for social justice and redistribution.24 Here we have a signal example: a set of international legal rules and sanctions that requires states to protect a form of property that prioritizes the profit imperative over access to essential goods, and that generates net wealth transfers to multinational companies based in the global North.
A right to medicines imbricated into this regime is plausibly regressive: it places significant strain on healthcare budgets, redistributes upwards, and provides medicines on terms largely dictated by one of the most profitable industries in the world. This right to medicines, in short, reflects and even intensifies a neoliberal approach to medicines. It mandates discrete individual relief, but rarely sees, much less disrupts, the underlying legal logics and structures that help produce radical health inequities.
The neoliberalism on display here is a soft form: courts do leave local legislatures free themselves to reorder the political economy of medicine. But when courts fail to articulate the right to health as having any necessary implications for political economy, they construct a picture of the right to medicines that, both conceptually and legally, sides with the prevailing order. This human rights abets not just neoliberal imaginaries, but also neoliberal legalities.
A different vision of human right is also possible. Medicines activists and their supporters have asked courts and other human rights bodies not merely passively to permit, but actively to encourage or even require states to intervene to promote a more just political economy. This is a vision of human rights with the potential to make medicines available more equitably, and also to begin to undermine the reach of the WTO’s rules. In a few notable cases, courts have embraced such claims. An anti-neoliberal human right to medicines is possible, in other words, and courts could play a role in it. But it can hardly be called likely, in part because human rights as a legal order has so far been constructed as if it has no necessary implications for the political economy that it helps to construct. If a better human rights is possible, a far darker one is, too. Corporations are also invoking human rights language and law, using claims to property or due process to try to preclude legislative majorities from controlling prices and limiting the power of patents—not entirely without success, as I will describe.
Human rights are no mere bystander in our neoliberal age. Human rights are inevitably entangled with neoliberal legality. The struggle for the meaning of human rights—as movement and as law—matters for those who wish to challenge the prevailing order, not only because it could help advance real change, but also because it could forestall it. The prevailing right to medicines embodies logics that undermine health equity, even if it also leaves room for committed legislatures to work around courts to create foundations for more equitable health systems. A model of human rights more adequate to our Gilded Age is also possible, one that would prompt and even direct legislatures to take such steps.
A more transformative human rights movement must go beyond simple attention to socioeconomic rights. It requires attention to the structural changes that are needed to reform our political economy, and to provide the infrastructure for fair provision, locally and globally, that neoliberal legality has steadfastly opposed. This revitalized movement would take its inspiration less from mainstream human rights than from its margins, and from the arguments and strategic savvy of those, like access to medicines advocates, who have grasped hold of pieces of the global logic of neoliberalism and begun successfully to challenge them.
Neoliberalism and Human Rights
What is the relationship between human rights and neoliberalism? The question first requires a working understanding of the two key terms. As David Harvey describes it, neoliberalism is the view that “human well-being can best be advanced by liberating individual entrepreneurial freedoms and skills within an institutional framework characterized by strong private property rights, free markets, and free trade.”25 Though often identified with a utopian economic project, properly understood, neoliberalism is a fundamentally political project, one that redefines the tools and contours of economic and social management—putting some on the side of free markets and others in the domain of impermissible regulation—in order to “reestablish the conditions for capital accumulation and to restore the power of economic elites.”26 As recent histories of neoliberalism stress, neoliberalism is less anti-government than a claim for a particular kind of governance: governance that protects market order from democratic demands, and that creates a right or privilege to accumulate for those empowered to wield capital.27
As an example of the fundamentally political nature of neoliberalism as well as its relation to governance consider the domain of “intellectual property.” Are intellectual property rights prerequisites of free markets in information, or government-granted monopolies that pervasively regulate everyday life, and intrude to benefit some market players over others? Mainstream economic and legal texts from the 1980s and 1990s cast stronger IP rights as the former. Strong IP rights formed part of the “Washington Consensus” and the core development teachings of institutions such as the World Bank and IMF, and were central pillars of new world trading order created in the 1990s. This led to an extraordinary wave of expansion in private IP rights around the world that, in turn, has had significant distributional effects. The move made it harder for people around the world to access basic necessities, including essential medicines. It also—not by accident—tends to advantage large firms over small, and incumbents over upstarts.28 There is also growing concern, including in mainstream economic circles, that the move has undermined economic efficiency, classically understood.29 Stronger IP rights were adopted around the world not because they were a tool of economic efficiency (though they were promoted as such at the time) but because they gave power to certain elite countries and companies, despite their social and economic costs.30
As a political project, neoliberalism has been extraordinarily successful, with influence far beyond intellectual property rights. Domestic and international policy and law have, in many areas, adapted to facilitate its program.31 In part as a result, inequality has grown dramatically more stark by many measures in recent years, particularly at the very top of the distribution.32 Welfare states have declined, generating dislocations and insecurities and a new “crisis of care.”33 Widespread experiences of precarity, stagnation, and powerlessness have also had palpable political effects in many parts of the world.34
Did human rights facilitate this? To explore this, we need a working definition of that term as well. As Philip Alston has pointed out, critics rarely directly confront the “polycentric nature of the human rights enterprise.”35 Human rights is at once a formal legal regime, a movement, and a universalizing mode of claims-making. The legal regime creates entitlements at both the national and international level, and is accompanied by institutions authorized to amend, interpret, and enforce these entitlements.36 In its discursive form, “human rights” simply designates a kind of universalizing claim: “I have a right.”37 Anyone can claim a right to this or that, and in that moment stage a kind of politics of disagreement, and demand an accounting.38 Finally, “human rights” also designates a globalized movement with dominant and dissident strands that has spanned decades, if not centuries. The power of “human rights” can be attributed in part to the productive interplay between these domains. The term names a relationship, a transit point, between claims, movements, and law.
So understood, does human rights abet neoliberalism, or give us tools to contest it? We now turn to that question, via an exploration of the contours of the right to medicines as it has emerged around the world, and particularly in Brazil and Colombia.
The Judicialized Right to Medicines
Brazil is known in international circles both for progressive health policies, such as a longstanding commitment to universal access to HIV medicines, and for its profound inequalities in access to healthcare and medicines.39 The 1988 Brazilian Constitution proclaims health as a fundamental social right, and by the mid-1990s, Brazilian NGOs and patients seeking access to HIV/AIDS medicine filed the first lawsuits seeking judicial enforcement of an individual right to medicines.40 Courts were receptive, so individuals needing other medicines too turned to the courts.41 They succeeded as well. Today, conservative estimates suggest that forty thousand people per year file suit in Brazilian courts seeking access to medicines and other specific health services.42 Plaintiffs win 80 to 90 per cent of the time, and the number of cases has grown explosively.43 For example, in just one state, Rio Grande do Sul, there were 1,126 right to health suits filed in 2002, 6,800 in 2006, 12,262 in 2008, and 17,025 in 2009, and fully 70 per cent of these cases sought access to medicines.44
Plaintiffs often seek access to drugs that are already on approved government lists, though experts disagree about whether this is a majority or minority of the overall claims.45 It is clear, however, that plaintiffs also frequently request drugs that the government has not agreed to provide as part of the public healthcare system, and that here too they are overwhelmingly successful.46 When evaluating claims, courts “almost universally” grant access to the medicines in question, even if they are very costly.47
Some of the medicines courts order the government to provide are, indeed, extraordinarily expensive. Among the most frequently requested medicines in court cases in Brazil in one dataset, which covered cases from 2002 to 2009 in Rio Grande do Sul, was peg interferon, a treatment for Hepatitis C, which cost $3,000 per month in Brazil.48 To put this figure in perspective, that is nearly ten times the monthly minimum wage there.
The budgetary impact of the right to medicines cases has unsurprisingly been significant. According to government figures, from 2010–2016, the federal government spent 4.4 billion reais ($1.4 billion) to comply with judicial decisions, with most of this going to provide medicines.49 This sum has risen sharply over time, along with the number of cases.50 In 2016 alone, the federal government spent 1.2 billion reais ($400 million) to satisfy judicial mandates.51 The bulk of suits for access to medicines arises at the state level, where data are harder to come by. But analysis has found that states and municipalities may be spending anywhere from 3 to 10 per cent of their health budgets to satisfy right to health cases, and as much as 22 per cent of their medicines budgets to fulfill judgments mandating access to medicines.52
Responding to concerns about the impact of these judgments on the healthcare system, in 2009, the Supreme Court of Brazil held hearings and issued an advisory opinion recommending that courts intervene only in a limited set of cases.53 It suggested that the government was obliged to provide drugs listed on the official government formulary or recommended by guidelines or clinical protocols, but that where drugs were not on the official list, the government was obliged to provide them only if they were approved by Brazilian regulators, no adequate alternative was available, and the treatment had been available for a significant time.54 In 2011, the legislature also revised the process for listing of drugs on the formulary to make it more fair and transparent, and also forbade the public provision of drugs not listed on the formulary.55 The administrative agency of the courts has also created guidelines for judges, recommending procedures such as consultation with doctors and pharmacists, to help ease case management and to protect the sustainability of the healthcare system.56
The impact of these reforms is not yet fully clear. Whether judges will follow recommended practices is in some doubt, particularly after a 2014 case in which the Supreme Court refused to follow its own advisory opinion, and mandated access to a treatment that cost more than $400,000 per year and had neither been approved in Brazil nor listed on the government formulary.57 And while legislative reforms have made the system for approving and listing medicines more fair and accountable, spending on medicines has continued steadily to rise.58 Recent reforms seem also to have had only modest impact on the cost of judicialization.59
Colombia has seen even more extensive litigation than Brazil.60 There, “more than 1.3 million lawsuits were filed between 1999–2014 demanding access to health care services, treatments, and pharmaceuticals.”61 Here, too, litigants are overwhelmingly successful, and have frequently obtained medicines excluded from the defined benefits package for insurers.62 The costs generated by these cases have also been substantial, reaching 1 per cent of GDP per year.63 In 2008, approximately 22 per cent of the total public pharmaceutical budget went to satisfy judgments for just seven drugs, most of which treated cancer.64
Critics of the Colombian cases have also provided initial evidence suggesting that the individuals benefitted are typically not among the poorest.65 In Colombia, too, the initial wave of judicialization triggered reforms. In 2008, the Constitutional Court issued a framework decision designed to curb the number of cases by prompting action from the executive, for example requiring it to update the basket of services and medicines in the defined benefits package.66 The decision helped prompt major new legislation that both affirmed a rights-based approach to access to medicines and healthcare and sought to impose cost-benefit criteria for the listing of provided services.67 The Constitutional Court, however, reviewed the law before it went into effect and concluded that the use of “a cost-efficiency rationale violated the government’s commitment to the right to health.”68 The government could not, the court suggested, ration medicines simply because of their cost.
The legislature responded with a revised law in 2015, providing public funding for all treatments except for those that are cosmetic or aesthetic; that lack scientific evidence regarding their safety or clinical efficacy; that are unapproved or experimental; and that are provided overseas.69 Colombia has also imposed increasingly strong price control measures in an effort to curb the budgetary impact of judicialization.70 This has significantly reduced the prices of individual medicines, but overall expenditures on medicines have risen precipitously, posing a serious challenge to the sustainability of the system.71 While court reforms initially appeared to reduce the rate of judicialization, the number of cases has since rebounded.72
Uruguay, Costa Rica, and Argentina have also seen significant, though less extensive, “judicialization.”73 Here, too, patients are frequently successful, even when they claim medicines that are not intended to be provided by the public system, or even approved for sale in the country.74 Again, significant sums are at stake, driven by the high cost of a small number of medicines.75
Though concentrated in Latin America, these cases are not limited to the region. In South Africa in 2002, the Constitutional Court ordered the state to provide women with treatment to prevent the transmission of HIV to their children.76 More recently, a High Court in India held that the government had a constitutional obligation to provide a child with medicine for a rare genetic disorder known as Gaucher’s Disease.77 The medicine cost $10,000 per month in India, and treatment is lifelong.78 For the court these facts were irrelevant: “No government can wriggle out of its core obligation of ensuring the right of access to health facilities for vulnerable and marginalized section[s] of society . . . by saying that it cannot afford to provide treatment for rare and chronic diseases.”79
What could it possibly mean to make states liable for providing medicines regardless of the price? The literature evaluating the impact of these right to medicines cases has yet to seriously confront a basic question—one that has been at the heart of the movement for access to medicines since its inception.80 Why are the medicines involved, or more accurately, some of the medicines involved, so profoundly expensive? It is common ground that the “exponential growth in costs” in Brazil “can be explained by a high concentration of cases demanding expensive patented drugs.”81 Almost 80 per cent of the total sum spent by the federal government to satisfy judgments for medicines in 2011 was spent on just 20 medicines, for fewer than 0.05 per cent of litigants.82 In Colombia, too, costs are driven overwhelmingly by a small number of expensive drugs: one-fifth of total spending on drugs in the country in 2008 went to cover the costs of just seven expensive drugs mandated by courts.83 This is consistent with the broader picture that we see in markets elsewhere, like the United States: The primary driver of medicines spending are newer, high priced medicines that are protected by patents and other forms of exclusivity.84
Why are these newer medicines so astronomically costly? Not because they are costly to make, but because producers enjoy monopoly rights. For example, a new breakthrough treatment for hepatitis C can be made for as little as $170, but the company holding the key patents priced it at $84,000 in the United States.85 This is, in fact, one of the core insights that fueled the access to medicines campaign: HIV medicines that were being sold for $10,000 to $15,000 a year (and that must be taken for life) could be sold for as little as $100 in the absence of monopoly.86 The treatment of millions of people with HIV in the global South has been, in fact, predicated on the use of cheaper, high-quality generic medicines, often imported from India or made locally.
Another example from Brazil is illustrative. One of the earliest drugs subject to extensive judicialization in Brazil is the anti-HIV drug Kaletra, made by the United States-based multinational firm Abbott.87 Kaletra is essential to basic HIV therapy, but the price was, and continues to be, a major issue for the Brazilian AIDS program. When it was added to the national program, Kaletra quickly came to absorb one third of its total medicines expenditures.88 Generics, though, could have been purchased for substantially less.89 After nearly a decade of sharp negotiations with Abbott, Brazil still paid almost twice the price for Kaletra that it would have paid if it purchased generic versions of the drug.90 Because of the scale of the universal AIDS treatment program, the government could have saved nearly $4 billion over just a few years had it purchased generic medicines.91 But it did not.
The Political Economy of Existing International Law
Why? The answer lies in the contemporary political economy of pharmaceuticals, as it has been shaped by international trade law and by the trade agendas of multinational companies and their affiliated governments, and particularly the United States. When negotiations began to create the new World Trade Organization in the 1980s, a set of multinational companies based in the United States—represented by the CEOs of several powerful pharmaceutical, entertainment, and software companies—joined together to lobby the United States, Europe, and Japan to write intellectual property law into the WTO.92 The proposal was simple and unprecedented: to link obligations on intellectual property to the global trading regime, and in the process, force developing countries to adopt strong IP laws if they wanted entry to the new regime. Because the WTO would have a new and powerful adjudicatory mechanism, developing countries would now also face trade sanctions if they violated their IP commitments. The companies succeeded in their campaign by appealing both to the self-interest of wealthy countries (because intellectual property is one of their main exports and a source of comparative advantage) and to a broader neoliberal account about the need for strong property rights to support the production of global public goods. Strong patent rights, the companies argued, are essential to the development of new medicines. At the time, more than fifty countries in the global South did not permit patents on medicines—as was typical for many northern countries, too, earlier on in their development.
The WTO’s Trade-Related Aspects of Intellectual Property Agreement (TRIPS) required all countries to introduce IP protections like those in the global North, including product patents on medicines.93 From the perspective of many economists, this condition was a scandal.94 Rather than following the “win-win” theory of comparative advantage, the logic here seemed to be either a simple rent transfer from South to North, or some kind of commitment to global public goods production. Both were predicted to strain the legitimacy of the global trading order.95
These predictions were prescient. Just a few years after the TRIPS Agreement came into effect, the issue of access to HIV/AIDS medicines roared onto the global stage. In 1996, new combination antiretroviral regimens were introduced in the global North, and dramatically decreased AIDS deaths there. But these same medicines were priced out of reach of almost everyone in the rest of the world, where more than 80 per cent of people living with HIV/AIDS lived. Activists mobilized around the issue and urged Indian firms to develop generic versions of anti-HIV drugs at a fraction of the cost of the patented drugs. Only after the patented price (around $25,000 a year) was brought down to the generic price—around $300 then, closer to $100 today—were the AIDS treatment programs that have since saved millions of lives created.96
It was in this crucible that health activists came to understand the implications of the TRIPS Agreement for the first time. TRIPS requires drug patents, and also allows countries to override those patents to make use of generic drugs. But the agreement is vague about the permissible conditions for overriding patents. For example, it requires “adequate” compensation and “reasonable” prior negotiation in the absence of emergency.97 Countries have been uncertain about how the terms and exceptions in TRIPS could be interpreted, and were pressured by the United States in particular to avoid any such measures. After intensive technical support and mobilizing by activists, several developing countries have issued compulsory licenses on AIDS medicines, but sometimes at a cost.98 When Thailand recently issued a spate of high-profile compulsory licenses, for example, the U.S. government and companies retaliated sharply—the United States by withdrawing certain trade preferences, and companies by withdrawing medicines from Thailand in protest.
The existing political economy of medicines, as this describes, is dominated by powerful pharmaceutical interests that have had a great deal of success in reshaping law and policy around the world. They have done this through a kind of squeeze play: by securing the passage of international agreements that mandate restrictive IP law in most of the world, and leveraging trade pressure from the United States and European Union to punish countries that seek to use flexibilities allowed by these same agreements.99
The result might be tolerable if TRIPS had the global public goods results that were claimed for it. But theory and facts suggest otherwise.100 The theory of patent-based R&D is, in essence, that we pay high prices for drugs and we get R&D in return. This system has only ever worked for wealthy countries (insofar as it has—there are problems here too) because a vast proportion of the world’s market resides in these countries and because R&D is expensive and the industry concentrated, leaving little room for small players who might focus on low-profit opportunities such as the diseases of the poor. Sub-Saharan Africa and India each comprises about 1 per cent of the world’s pharmaceutical market.101 All of Latin America makes up less than 5 per cent of the world’s market.102 And about 45 per cent of the world market is located in the United States alone, which has few mechanisms to constrain drug prices.103
It is not then a surprise to hear comments like the one recently made by the CEO of Bayer, when addressing the implications of a decision in India to override a patent on a Bayer cancer drug: “Is this going to have a big effect on our business model? No, because we did not develop this product for the Indian market. . . . We developed this product for Western patients who can afford this product, quite honestly.”104 The Onion captured the logic of the prevailing system even better, in a recent headline that reads: “Experts: Ebola Vaccine At Least 50 White People Away.”105 As James Surowiecki recently put it, we should not be surprised that drug companies invested nothing in Ebola for decades:
Diseases that mostly affect poor people in poor countries aren’t a research priority, because it’s unlikely that those markets will ever provide a decent return. So diseases like malaria and tuberculosis, which together kill two million people a year, have received less attention from pharmaceutical companies than high cholesterol. Then, there’s what the World Health Organization calls “neglected tropical diseases,” such as Chagas disease and dengue; they affect more than a billion people and kill as many as half a million a year. One study found that of the more than fifteen hundred drugs that came to market between 1975 and 2004 just ten were targeted at these maladies. And when a disease’s victims are both poor and not very numerous that’s a double whammy. On both scores, a drug for Ebola looks like a bad investment: so far, the disease has appeared only in poor countries and has affected a relatively small number of people.106
Effective Ebola vaccines and treatments will be the result not of our dynamic private sector, but of substantial investment by government, and by the National Institutes of Health in particular.107 Government, it turns out, is a major funder of not only basic research, but also drugs for neglected diseases, because markets predictably fail to serve the millions who suffer from these diseases.108
The conventional theory that supports the exclusive rights approach to information production is based upon the idea that markets will do better than governments in guiding decisions about what to produce, and how much to spend.109 But markets only can do this well if prices are able to adequately track the relevant form of social value. There are deep debates about exactly how to characterize that value when it comes to global health.110 But what is clear is that a market-led system for medicines will not—and cannot, given existing levels of inequality—produce medicines in a way that corresponds to global public health needs, or that redresses the extreme inequality that characterizes health outcomes in our world.111
Free markets and strong IP in the domain of global health thus have predictably inequitable results. They link innovation and access to high prices that the poor cannot pay—and that governments are often unwilling to pay for on their behalf. The problems that this model produces for the global poor, moreover, are intensified by domestic inequality, which has intensified in the wake of neoliberalism. One of the reasons that pharmaceutical companies price drugs at very high levels even in relatively poor countries is that high prices in these countries can be profit-maximizing. Charging high prices to a small percentage of wealthy patients will produce greater returns than charging low prices to a large number of the poor, if inequality within a country is high.112 The more unequal a society is, the more likely this is to be the case.113
A Progressive Right to Medicines?
The contemporary political economy of medicines is designed in a manner that has deep maldistributive implications: it prioritizes the development of profitable medicines, and thus of medicines that treat diseases of the North. It is also designed to regularly deny the poor, particularly in the global South, access to new medicines that are developed because it is hard to segment the markets of the poor and rich. The former become collateral damage to a pricing strategy focused on the latter.
Does human rights offer any serious threat to this logic? Plausibly, right to medicines cases not only do not dislodge the contemporary political economy of medicines, but they put that logic on steroids: they impose a legal obligation on governments to provide high priced medicines, regardless of the cost. At least one court has even held that the right to health means the right to a particular brand of drug, if a doctor prescribes it.114 Any reckoning with the political economy that produces high prices in developing countries or with the failure to develop drugs for neglected diseases is relegated to other branches of government.
The right to medicines could, though, be understood differently. Presented with arguments made visible here, about the nature of the relation between political economy and equitable access to medicines, courts might ask, or even require, governments to intervene. Consider, for example, the campaign built by Brazilian activists to create a more sustainable and equitable AIDS treatment program by demanding that the government override patents to reduce the costs of HIV drugs. Right to health arguments first were deployed in campaigns targeted at the executive that met with limited success.115 In frustration, activists filed a lawsuit demanding that the government issue a compulsory license on Kaletra, and showing that the move would reduce costs substantially, for a medicine that, at the time, took up 30 per cent of the national expenditure on HIV/AIDS medicines.116 The aim, as activists put it, was to seek “alternative forms of integration that contrast with the logic of trade and financial liberalization prevailing in the economic agreements currently being negotiated” in the international arena.117
A Brazilian court, however, rejected the claim on preliminary analysis, questioning the ability of local companies to make the generic drug and citing the possibility that the United States would retaliate against the country in trade terms.118 The coalition, working with international experts, produced analysis to show that the drugs could indeed be produced locally, and returned to the court. The court, though, sat on the case and still today has not issued another decision.119
The same coalition devised another constitutional challenge thereafter to an aspect of Brazil’s patent law, seeking to invalidate a range of key patents on HIV/AIDS and other medicines that cost the government billions of dollars.120 They argued that retrospectively awarding so-called “pipeline” patents—on old inventions that TRIPS suggested must be permitted once the treaty was implemented—violated the constitutional obligation that intellectual property serve the “economic and technological interests of the country.”121 Patents are intended to stimulate innovation, but you cannot generate innovation by giving retrospective protection, as they pointed out. The group convinced the Prosecutor General to lodge an appeal on the matter in the Supreme Court, where it has languished since 2009.122
AIDS activists in Colombia made similar efforts, collaborating with international activists to try to obtain, and then force, a compulsory license on Kaletra. Activists involved recognized that insurance companies were routinely violating their obligations to provide HIV/AIDS medicines, but argued that judicialization alone could not provide a solution. High prices, they noted, worked against the expansion of coverage, and led insurance companies to try to avoid paying by barraging patients with paperwork or forcing them to go to court.123 Patients ended up spending a week a month battling ever-changing bureaucratic requirements imposed by insurers, and going to court for orders mandating access to their antiretrovirals.124 Overwhelmed, they would drop out of treatment as a result.125 The fundamental barriers to access to medicines in Colombia, activists contended, involved “intellectual property regulations and the way they have been exported to developing countries.”126
Pointing out that Kaletra absorbed one quarter of the HIV/AIDS medicines budget in the country, and that generics could be procured abroad for one-third the price, they appealed to the executive to permit generics by issuing a compulsory license in accordance with both Colombian and international law.127 After two years of meetings, negotiations, and protests—chanting “For the Right to Health, No More Patents”—the government agreed to explore the option.128 But it then refused to issue a license, citing the reason given by Abbott. The drug was available through insurance schemes so that patients themselves did not need to pay; the compulsory license was thus not in the public interest.129 Activists viewed the rejection as the outworking of pressure from the United States, in particular related to the pending United States-Colombia FTA, which was awaiting approval in the United States.130
Stymied in their appeal to the executive, activists asked the courts to require a compulsory license, to vindicate the collective right “to an infrastructure of services ensuring public health.”131 They argued that the collective entitlement to universal healthcare required lower prices to ensure sustainability of the system and that patients in fact received the medicines to which they were entitled.132 The court rejected their request, implying (incorrectly) that move was inconsistent with international IP treaties.133 It did, though, also deliver activists a modest victory: it ordered the government to enforce the price controls that existing law permitted. The state had an obligation to provide healthcare under the constitution, the court reasoned, so it was also required to enforce its price controls, because the savings—though they would not reach individual patients—would “translate into additional resources for the entire health system.”134 The ruling brought the price down by around 50 per cent, though Kaletra still cost twice what it might have had generics been made available.135
Both cases show the difficulty that activists face when they directly challenge the existing political economy of medicines. Because human rights have generally been conceived of as having no necessary relation to arrangements of political economy, decisionmakers are often perplexed by their claims, and misapprehend the political economic order that they bring into view. The Colombian court’s response, however, begins to sketch another future. While rejecting a mandatory license, it nonetheless affirmed that the right to health required reasonable prices, beginning to articulate that human rights and the design of a market order have something to do with one another—something that the Brazilian courts have so far assiduously rejected. The Colombian Constitutional Court similarly recognized the importance of affordability to the right to health when it rejected companies’ arguments that a recent price control law interfered with constitutional protections for economic freedom.136
Note, though, a tension that courts that accept price controls as measures intended to protect the right to medicines will face. In response to price controls, companies may threaten to refuse to sell their medicines at all, either pushing prices up, or denying patients access. If stringent price controls mean companies refuse to sell, they might be seen as in tension with the constitutional obligation to provide medicines. Companies in fact made this point in their challenge to Colombia’s price controls; the court responded by simply denying that companies would make good on their threats.137 Access to medicines activists take a different approach. They focus on breaking monopolies, because this gives governments greater leverage: they can back up price negotiations by threatening to put patents rather than patients at risk. If companies refuse to sell, governments can find generic competitors who will. Price controls alone, in other words, may not provide an adequate answer to the challenges that the current political economy of medicines poses to health and equity.
Courts in other countries, though, have gone further, concluding that the right to health can have implications for monopoly rights themselves. Consider, for example, two recent path-breaking cases, one in India and one in Kenya.138 In Roche v. Cipla, a high court in India refused to issue an interim injunction in a patent case against a generic drug company, explicitly citing the right to life (which is the basis for the right to health) in the Indian Constitution. Noting the significant price implications of barring the generic cancer drug from the market, the court acknowledged that “the Courts have to tread with care [when] lifesaving drugs are involved.”139 It also concluded that it could not
be unmindful of the right of the general public to access lifesaving drugs which are available and for which such access would be denied if the injunction were granted. The degree of harm in such eventuality is absolute; the chances of improvement of life expectancy; even chances of recovery in some cases would be snuffed out altogether, if injunction were granted. Such injuries to third parties are un-[compensable]. Another way of viewing it is that if the injunction in the case of a lifesaving drug were to be granted, the Court would in effect be stifling Article 21 [which protects the right to life] so far as those [who] would have or could have access to [the drug in question are concerned.140
Here, human rights shaped the court’s application of India’s patent law, precisely because enforcing the patent in question would have done significant harm to access to medicines.
The Kenyan case is more assertive still. There, local AIDS activists urged that a recent “anti-counterfeiting law” that would have impeded access to legitimate, high-quality generic medicines in Kenya violated the right to health and life. The law purported to target unsafe counterfeit medicines, but its definition of “counterfeit” swept in safe and high-quality generic medicines. Indeed, its definition was so broad that it treated as counterfeit and medicine that infringed a patent in Kenya “or elsewhere.”141
The High Court sided with petitioners. It first announced, interpreting the relatively new constitutional right to health, that “any legislation that would render the cost of essential drugs unaffordable to citizens would thus be in violation of the state’s obligations under the Constitution.”142 It noted that the law’s purpose—”the protection of . . . the general public from substandard medicines” could not be squared with the broad preclusion of medicines that simply violated patents.143 The court concluded that the law unjustifiably posed great risk to the availability of generic medicine in the country, and struck it down. In a key passage, it reasoned that “While . . . intellectual property rights should be protected, where there is the likelihood, as in this case, that their protection will put in jeopardy fundamental rights such as the right to life . . . , I take the view that they must give way to the fundamental rights of citizens in the position of the petitioners.”144 Activists have also developed more sophisticated versions of such claims, asking courts to weigh and illuminate the key policy issues with regard to patents—namely, their comparative impact on access and innovation—before acting. The South African Treatment Action Campaign (TAC), for example, intervened as an amicus in a recent patent dispute between two companies in South Africa with a very sophisticated version of the argument that prevailed in the Indian case (and citing the Kenyan one). TAC urged the court to construe the national patent law “through the prism of the Constitution” and in particular the right to health.145 It urged the court to interpret the right to health to create a procedural burden for companies seeking injunctions in patent cases. These companies should, TAC argued, have to put forth evidence about the impact of the injunction on access to medicines, and should also be allowed to lodge evidence about the importance of such an injunction to the protection of profits needed to recoup R&D investments specific to South Africa.146
TAC had useful precedent to draw upon. In 2005, the South African Constitutional Court had rejected a challenge to a price control law, with one Justice stating that “preventing excessive profit-taking from the manufacturing, distribution, and sale of medicines is more than an option for the government. It is a constitutional obligation, flowing from its duties under section 27(2),” which protect the right to health.147 TAC argued that the right to health required the courts to ensure that the patent law did not excessively reward drug companies by permitting them high prices that could not be justified by investment in innovation. The lower court was, however, unconvinced—indeed, uncomprehending: “I cannot see,” the judge declared, how “the prism of the Constitution comes into play so as to deny [the] right to enforce [a] patent.”148
There is a deeper point here, one that is central to scholarship on law and political economy.149 Most courts have resisted the idea that the right to health may have implications for the permissible shape of patent law because prevailing legal logics—visible in human rights law as elsewhere—construct markets as existing in a separate realm, the realm that some would call “private” instead of “public” law. But as legal realists recognized long ago, the “free market” is constructed and enforced by the state. And courts are always inevitably intervening in markets, even when they frame their interventions as leaving markets alone.150 Courts and other actors engaged in elaborating the right to medicines decide when they reject claims that owners of patents have a duty not to injure others, just as they act when they affirmatively intervene to mandate price controls or to preclude patent injunctions that put lives at risk.
As these cases show, there are many different ways that courts can seek to intervene in the political economy of medicines. Some are more assertive—striking laws down on constitutional grounds, as in Kenya. Less ambitiously, courts can interpret the common law of remedies or order the executive to enforce a law on the books, as in India and Colombia. Dialogic approaches are possible, too: courts might invite legislatures to consider invoking tools like compulsory licensing, as the Peruvian Constitutional Court recently did.151 Or they might order legislatures to consider such options instead, elaborating a more assertive but still process-oriented relation between the right to health and the political economy of medicines.
All of this can draw some support from the Geneva-based human rights system, where activists have also advocated the creation of analytics to help their claims along. Special Rapporteurs—including one, Anand Grover, who has long been a key figure in the access to medicines movement—have argued that to fulfill their human rights obligations, developing countries should or even must use TRIPS flexibilities.152 They have urged companies to commit resources to innovation for neglected diseases, and even offered sophisticated political economy critiques of for-profit research models.153 While Special Rapporteur on the Right to Food, for example, Olivier de Schutter argued that the right to “enjoy the benefits of scientific progress and its applications” (in Article 15 of the International Covenant on Economic, Social and Cultural Rights) has implications for not just the amount but also the kind of scientific research that states support.154 Because “profit driven research serves the needs of the high-value segments of the markets, while neglecting the real needs of the poorest and most marginalized groups,” he noted, a “strong role for public investment in research” is needed to compensate.155
Lit up here is the possibility of a human rights model that restructures our political economic order. In place of market incentives and willingness to pay, it insists upon a public and political priority for equity, an in accordance with health need rather than profit imperatives. It has not yet succeeded, precisely because it challenges the mainstream constructions—visible in the right to medicines cases—that see the right to health as in no deep tension with the prevailing political economy. But the dissident strand does have the potential to work significant change. Were local courts to follow it, they could begin to interpret the right to health and life in ways that have direct implications for patent law, and for the use of TRIPS flexibilities such as compulsory licenses or price controls where these mandates are necessary to protect health and health equity. These could have important implications locally, and also that reverberate through the global trade system. WTO panels are plausibly allowed, even required, to take human rights law into account, and would be put in an extraordinarily difficult position if asked to interpret WTO agreements in a manner that required countries to violate their own constitutional commitments to the right to health.156 New IP treaties that ratchet up protections would be harder to conclude in such a world as well; states would be signing agreements that violated their own constitutions.
This is a vision of human rights that is anti-neoliberal, that seeks—whether dialogically or substantively—to intervene to construct a more just political economy, to secure not just an individual right to medicines but also the infrastructure necessary to make medicines available more equitably for all.
By engaging in this domain, activists are also forestalling a far darker future, where claims of human rights are used to expand or entrench rights of intellectual property or systems of market ordering.157 Human rights law offers footholds for companies to argue that a neoliberal economy is not just permissible, but mandated, as companies in Colombia recently did when they challenged price controls. The International Covenant on Economic Social, and Cultural Rights declares that “everyone” has the right to “benefit from the protection of the moral and material interests resulting from any scientific, literary or artistic production of which he is the author.” UN human rights institutions have so far rejected the view that there is a human right to intellectual property per se, concluding that there are many ways other than property rights that authors can be recognized and compensated, and that corporations cannot be the bearers of human rights.158 But other human rights bodies have decided otherwise. Most prominently, the European Court of Human Rights, interpreting Article 1 Protocol 1 of the European Convention on Human Rights (which explicitly declares property a human right), has concluded that intellectual property rights—including those held by corporations—are protected under the European Convention.159 Expansions in this direction could rework human rights in extraordinary ways, rendering it a means to demand full compensation when governments override patents to protect the right to health, or granting companies extensive procedural rights that would undermine the ability to develop legal regimes that contest the neoliberal framework. This would be the apotheosis of a neoliberal human rights—rendering neoliberalism itself a kind of human right. That this approach too has made some gains reveals how contested, and important, the domain of human rights remains for those who seek to challenge our existing order.
—————————
It is right to criticize a certain mainstream of human rights—here, considered not just as movement but also as law—for failing to confront matters of political economy. Human rights is not, nor could it be, a mere bystander in struggles over neoliberalism. Rather, it is a sphere of action and conflict, one in which “the economy” is not merely present but constructed. If human rights is to do more than nip at the heels of neoliberalism, though, it must not merely mainstream or judicialize socioeconomic rights, but take on questions of political economy. It must challenge neoliberal logics that produce scarcity and inequality, and articulate claims to public prerogatives and infrastructures—reordering the relation between imperium and dominium, in Slobodian’s terms—that facilitate public and democratic power.
Of course, there is no guarantee that such a human rights can succeed. Nor is there reason to think that courts should be the sole, or even privileged destination for such claims. Courts are not even plausible destinations for some claims important to a more egalitarian approach to medicines, such as the demand that we move away from a market-driven system for allocating health research. (Could plaintiffs go to court seeking that a government create a serious R&D program, with a priority for the poor? The case is hard to imagine—though we might imagine courts demanding in “dialogic” fashion that governments have a plan for R&D that takes human rights concerns into account.160) A revised human rights would not ignore courts—for there the battle can be lost, if never won—but must also be attentive to the need to build a broader politics, and structures of political accountability, that are needed to achieve a more ambitious vision of justice at a global scale.161
This is far from the mainstream human rights that Klein, Moyn, and Marks critique, but glimmers of its potential are present in forms of human rights practice, particularly at the periphery, that exist beyond their view. It is in these marginal places that hope for human rights lies, and to these places that we should look if we want to build a human rights adequate to our times.
NOTES
Special thanks to Natália Pires de Vasconcelos and Ximena Benavides Reverditto, who provided excellent research assistance and help accessing and translating the sources cited here that are not available in English.
- Naomi Klein, The Shock Doctrine: The Rise of Disaster Capitalism (New York: Picador, 2007), 147.
- Ibid.
- Susan Marks, “Human Rights and Root Causes,” Modern Law Review 74, no. 1 (January 2011): 71.
- Ibid., 59.
- As Marks points out, the contemporary market system creates these results “not just contingently but necessarily, as part of its logic.” Ibid., 69.
- Ibid., 75.
- Samuel Moyn, Not Enough: Human Rights in an Unequal World (Cambridge, MA: Harvard University Press, 2018).
- Ibid., 216.
- Ibid.
- For critiques in this direction, see Peter Rosenblum, “When Splitters become Lumpers: Pitfalls of a Long History of Human Rights,” LPEBlog.org, August 10, 2018, accessed September 6, 2018, https://lpeblog.org/2018/08/10/when-splitters-become-lumpers-pitfalls-of-a-long-historyd-of-human-rights/#more-879; Julieta Lemaitre, “The View from Somewhere: On Samuel Moyn’s Not Enough,” LPEBlog.org, July 9, 2018, accessed September 6, 2018, https://lpeblog.org/2018/07/09/the-view-from-somewhere-on-samuel-moyns-not-enough/
- The access to medicines movement was not led by mainstream human rights organizations, and has not relied centrally on human rights law. But many of the leading groups in the access to medicines movement speak in the language of human rights, for example demanding “patient rights, not patent rights.” These include the Treatment Action Campaign, HealthGAP, ACTUP, the Lawyers Collective in India, and Médecins Sans Frontières. Some mainstream human rights organizations have also supported aspects of the campaign. See, for example, the work of the health and human rights division of Human Rights Watch, accessed August 22, 2018, https://wwwd.hrw.org/topic/health/hiv/aids-and-tuberculosis. Some of the most meaningful early cases of “judicialization” came from HIV/AIDS organizations that were central to the access to medicines movement. See Amy Kapczynski and Jonathan M. Berger, “The Story of the TAC Case: The Potential and Limits of Socio-Economic Rights Litigation in South Africa,” in Human Rights Advocacy Stories, ed. Deena R. Hurwitz and Margaret L. Satterthwaite (New York: Thomson Reuters/Foundation Press, 2009), 43–79 (describing the Treatment Action Campaign’s role in the leading South African case, providing anti-HIV medicines to pregnant women); Gabriela Costa Chaves, Marcela FogaÀ’Àa Vieira, and Renata Reis, “Access to Medicines and Intellectual Property in Brazil: Reflections and Strategies of Civil Society,” Sur: International Journal on Human Rights 5, no. 8 (June 2008): 164–66 (describing the role of AIDS activists and organizations in the earliest cases of judicialization in Brazil).
- See Mariana Mota Prado, “The Debatable Role of Courts in Brazil’s Health Care System: Does Litigation Harm or Help?,” Journal of Law, Medicine and Ethics 41, no. 1 (Spring 2013): 124–37; João Biehl, Mariana P. Socal, and Joseph J. Amon, “The Judicialization of Health and the Quest for State Accountability: Evidence from 1,262 Lawsuits for Access to Medicines in Southern Brazil,” Health & Human Rights 18, no. 1 (June 2016): 211.
- Everaldo Lamprea, “The Judicialization of Health Care: A Global South Perspective,” Annual Review of Law and Social Science 13 (2017): 431, 440.
- Ottar Mæstad, Lise Rakner, and Octavio L. Motta Ferraz, “Assessing the Impact of Health Rights Litigation: A Comparative Analysis of Argentina, Brazil, Colombia, Costa Rica, India, and South Africa,” in Litigating Health Rights: Can Courts Bring More Justice to Health?, ed. Alicia Ely Yamin and Siri Gloppen (Cambridge: Harvard Law School, 2011), 273; LucÀ1Àa Berro Pizzarossa, Katrina Perehudoff, and José Castela Forte, “How the Uruguayan Judiciary Shapes Access to High-Priced Medicines: A Critique through the Right to Health Lens,” Health and Human Rights 20, no. 1 (June 2018): 93–105. In the global North, courts have tended to conceive of constitutional rights as imposing primarily procedural requirements, outside of narrow settings such as the prison context. See Colleen M. Flood and Aeyal Gross, eds., The Right to Health at the Public/Private Divide: A Global Comparative Study (New York: Cambridge University Press, 2014).
- Moyn himself suggests that access to medicines is one of very few domains where human rights may claim to “have had some salutary effects in framing claims and even in promoting better outcomes.” Samuel Moyn, “A Powerless Companion: Human Rights in the Age of Neoliberalism,” Law and Contemporary Problems 77, no. 4 (2015): 165.
- Octavio Luiz Motta Ferraz, “The Right to Health in the Courts of Brazil: Worsening Health Inequities?,” Health and Human Rights 11, no. 2 (December 2009): 33–34; Octavio Luiz Motta Ferraz, “Moving the Debate Forward in Right to Health Litigation,” Health and Human Rights 18, no. 2 (December 2016).
- Alicia Ely Yamin, Oscar Parra-Vera, and Camila Gianella, “Colombia: Judicial Protection of the Right to Health: An Elusive Promise?,” in Litigating Health Rights, 114–16 (providing data, and describing and citing others who take this view); David Landau, “The Reality of Social Rights Enforcement,” Harvard International Law Journal 53, no. 1 (Winter 2012): 202–03.
- Daniel M. Brinks and Varun Gauri, “A New Policy Landscape: Legalizing Social and Economic Rights in the Developing World,” in Courting Social Justice: Judicial Enforcement of Social and Economic Rights in the Developing World, ed. Varun Gauri and Daniel M. Brinks (Cambridge: Cambridge University Press, 2008), 303, 337.
- João Biehl et al., “Between the Court and the Clinic: Lawsuits for Medicines and the Right to Health in Brazil,” Health and Human Rights 14, no. 1 (June 2012): 36–52.
- See Ole F. Norheim and Siri Gloppen, “Litigating for Medicines: How Can We Assess Impact on Health Outcomes?,” in Litigating Health Rights, 304–30.
- Ibid., 304–06 (providing a framework for systematically evaluating the direct impacts of medicines cases, and suggesting that a South African case that mandated access to a very cheap medicine to prevent mother-to-child transmission of HIV had equity benefits, while the Latin American cases likely had a negative effect on equity).
- Daniel M. Brinks and Varun Gauri, “The Law’s Majestic Equality? The Distributive Impact of Judicializing Social and Economic Rights,” Perspectives on Politics 12, no. 2 (June 2014): 375–93; Aquiles Ignacio Arrieta-Gómez, “Realizing the Fundamental Right to Health through Litigation: The Colombian Case,” Health and Human Rights 20, no. 1 (June 2018): 133–45; Everaldo Lamprea, Lisa Forman, and Audrey R. Chapman, “Structural Reform Litigation, Regulation and the Right to Health in Colombia,” in Comparative Law and Regulation: Understanding the Global Regulatory Process, ed. Francesca Bignami and David Zaring (Northampton, MA: Edward Elgar Publishing, 2016), 350–51; Yamin, Parra-Vera, and Gianella, “Colombia,” 119, 128.
- Alicia Ely Yamin, “Power, Suffering, and Courts: Reflections on Promoting Health Rights Through Judicialization,” in Litigating Health Rights, 365. Scholars have also argued that the implications of these cases would be more progressive if courts engaged more broadly with health policy, and relied on remedies that were more structural than individualized. Florian F. Hoffmann and Fernando R. N. M. Bentes, “Accountability for Social and Economic Rights in Brazil,” in Courting Social Justice, 145; Landau, Reality of Social Rights Enforcement, 246–47.
- Quinn Slobodian, Globalists: The End of Empire and the Birth of Neoliberalism (Cambridge, MA: Harvard University Press, 2018), 16.
- David Harvey, A Brief History of Neoliberalism (Oxford: Oxford University Press, 2005), 2.
- Ibid., 19.
- Slobodian, Globalists.
- See Yochai Benkler, “Intellectual Property and the Organization of Information Production,” International Review of Law and Economics 22, no. 1 (July 2002): 81, 83.
- Michele Boldrin and David K. Levine, Against Intellectual Monopoly (Cambridge: Cambridge University Press, 2008); Richard Posner, “Why There Are Too Many Patents in America,” The Atlantic, July 12, 2012, accessed August 22, 2018, http://www.theatlantic.com/business/archive/2012/07/why-there-are-too-many-patents-in-america/259725/
- Susan K. Sell, Private Power, Public Law: The Globalization of Intellectual Property Rights (Cambridge: Cambridge University Press, 2003); Peter Drahos and John Braithwaite, Information Feudalism: Who Owns the Knowledge Economy? (New York: New Press, 2002).
- See, for example, Andrew Lang, World Trade Law After Neoliberalism: Re-Imagining the Global Economic Order (Oxford: Oxford University Press, 2011), and the special issue of Law and Contemporary Problems 77, no. 4 (2014), on law and neoliberalism, accessed August 22, 2018, http://scholarship.law.duke.edu/lcp/vol77/iss4/
- See Thomas Pikkety, Capital in the Twenty-First Century, trans. Arthur Goldhammer (Cambridge, MA: Harvard University Press, 2014).
- Nancy Fraser, “Contradictions of Capital and Care,” New Left Review 100 (July–August 2016): 99–117.
- See Wolfgang Streeck, How Will Capitalism End?: Essays on a Failing System (New York: Verso: 2017); Patrick Bond, afterword to the new edition of “South Africa Faces its `Faustian Pact’: Neoliberalism, Financialisation and Proto-Fascism,” in Bond, Elite Transition: From Apartheid to Neoliberalism in South Africa (London: Pluto Press: 2014).
- Philip Alston, “Does the Past Matter? On the Origins of Human Rights,” Harvard Law Review 126, no. 7 (May 2013): 2045.
- One of the clear ambiguities in how we talk about human rights has to do with how and whether we understand domestic constitutional rights claims to be “human rights” claims. Here, I speak both of human rights law in international treaties, and also at the national level in constitutions that protect the right to health. For certain purposes, we might want to separate domestic constitutional protections from “human rights,” understood in a more transnational manner. But particularly where constitutions are outward looking and protect socioeconomic rights, there are reasons to encompass both in our understanding of human rights.
- With thanks to Alice Miller, who has memorably termed these “t-shirt rights,” and Tom Keenan, who has long described human rights as marking a form of discursive claim. See Thomas Keenan, Fables of Responsibility: Aberrations and Predicaments in Ethics and Politics (Stanford: Stanford University Press, 1997), 154–74.
- See Jacques Rancière, Disagreement: Politics and Philosophy, trans. Julie Rose (Minneapolis: University of Minnesota Press, 2004); Claude Lefort, “Politics and Human Rights,” in The Political Forms of Modern Society: Bureaucracy, Democracy Totalitarianism, ed. John B. Thompson, trans. Alan Sheridan (Cambridge: MIT Press, 1986).
- Biehl, “Between the Court and the Clinic,” 37.
- ConstituiÀ’Àão Federal [C.F.] [Constitution] art. 6 (Braz.) (“Health is the right of all persons and the duty of the State”). Chaves, Vieira, and Reis, “Access to Medicines and Intellectual Property,” 164–66.
- Danielle da Costa Leite Borges, “Individual Health Care Litigation in Brazil through a Different Lens: Strengthening Health Technology Assessment and New Models of Health Care Governance,” Health and Human Rights 20, no. 1 (June 2018): 150.
- For the forty-thousand figure, see Octavio L. Motta Ferraz, “Brazil: Health Inequalities, Rights, and Courts: The Social Impact of the Judicialization of Health,” in Litigating Health Rights, 76–102, esp. 85 and fig. 4.3. The Brazilian government reported in 2014 that there were around 400,000 such lawsuits total in Brazil filed by that date. See Borges, “Individual Health Care Litigation in Brazil,” 147–62, 150.
- See Biehl at al., “Between the Court and the Clinic,” 46; Biehl, Socal, and Amon, “Judicialization of Health,” 211; Daniel Wei L. Wang, “Right to Health Litigation in Brazil,” 623–24. See Ferraz, “Brazil: Health Inequalities,” 82 (noting that the number of federal cases increased five-fold from 2005 to 2009).
- Biehl et al., “Between the Court and the Clinic,” 40. For additional evidence on the growth of judicialization in Brazil, see Biehl, Socal, and Amon, “Judicialization of Health,” and João Biehl, “Patient-Citizen-Consumers: Judicialization Of Health and Metamorphosis of Biopolitics,” Lua Nova 98 (2016): 77.
- Biehl et al. report that in their sample the majority of requests are for approved drugs. See Biehl et al., “Between the Court and the Clinic,” 48 (“Two-thirds of the drugs requested by plaintiffs in our study were on governmental pharmaceutical distribution lists.”). Wang concludes, citing contrary studies, that “right to health litigation is mainly driven by individual claims for new health technologies, especially drugs, which have not been incorporated in the national public health system’s (SUS) pharmaceutical policy.” See Wang, “Right to Health Litigation in Brazil,” 619–20 (referencing studies that put the rate between 38 per cent and 92 per cent in different states, with most states at the higher end). Wang suggests that the discrepancy has to do with methodological differences. These estimates may also not consider the more complex question of whether the drugs being claimed are for an approved indication. Drugs are approved by indication, but an approved drug can be prescribed for nonapproved indications, for which there is neither substantial evidence nor regulatory approval. According to Wang, many claims involve approved drugs, but unapproved indications (621, citing a study putting the number of claims for unapproved purposes at 81 per cent).
- Wang, “Right to Health Litigation in Brazil,” 619–21.
- Biehl et al., “Between the Court and the Clinic,” 47. The only exception in Brazil noted in the literature is a case seeking drugs for four children with Gaucher’s disease. The drugs cost $250,000 per year for each child, with lifelong treatment required. This claim was denied when the state showed that did not have available the necessary funds. Hoffmann and Bentes, “Accountability for Social and Economic Rights,” 123. Keep reading for a blockbuster case that in fact ordered these drugs to be provided, not in Brazil, but in India. Hoffman and Bentes also cite several cases where medicines or interventions were denied as not sufficiently effective (123–24).
- Biehl et al., “Between the Court and the Clinic,” 45 tbl. 3; see also Hoffmann and Bentes, “Accountability for Social and Economic Rights,” 122–23 (noting that early claims were for expensive anti-HIV drugs, and today claims “cluster[] around a number of medicines classified as exceptional by the [Unified Health System] and linked to chronic conditions such as Crohn’s disease, chronic viral hepatitis C, severe kidney disease, hypertension, and heart disease”).
- Victor Maciel, “Ministro da Saúde apresenta desafios da judicializaÀ’Àão, em Portugal,” Agencia Saude, Ministry of Health, Brazil, 2017, accessed August 29, 2018, http://portalms.sauded.gov.br/noticias/agencia-saude/28137-ministro-da-saude-apresenta-desafios-da-judicializacao-emd-portugal; Bruno de Pierro, “Demandas crescentes,” Pesquisa FAPESP 252, February 2017, accessed August 29, 2018, http://revistapesquisa.fapesp.br/2017/02/10/demandas-crescentes/
- In 2009, for example, the federal government paid $83 million to satisfy judicial mandates to provide medicines. Ferraz, “Brazil: Health Inequalities.” This was a relatively small portion of the federal health budget (0.4 per cent), but a more sizable portion of overall federal expenditures on medicines (1–4 per cent). Mæstad, Rakner & Ferraz, “Assessing the Impact,” 290.
- Maciel, “Ministro da Saúde apresenta.”
- Ferraz, “Brazil: Health Inequalities,” 83 (states and municipalities spent around 8 per cent of their health budgets to satisfy right to medicines cases in 2009); Wang, Right to Health Litigation in Brazil, 627–28 (providing sources showing that the percent of healthcare budgets spent on satisfying right to health judgments was 3 per cent in the state of Minas Gerais in 2013; 5 per cent in the state of Sao Paolo in 2010; and 10 per cent in the city of Sao Paolo in 2011); Biehl et al., “Between the Court and the Clinic,” 47 (in 2008, in one state, Rio Grande do Sul, 22 per cent of all medicines expenditures was spent on court-ordered medicines, constituting 4 per cent of the projected health budget).
- See Wang, “Right to Health Litigation in Brazil,” 631–32. See also Mariana Motta Prado, “Provision of Health Care Services and the Right to Health in Brazil,” in The Right to Health, ed. Colleen M. Flood and Aeyal Gross, 341 (noting also that the decision is not binding on the lower courts).
- See Wang, “Right to Health Litigation in Brazil,” 634.
- Ibid., 638–39. The government’s hope is that judges will largely defer to its determinations. Ibid., 639, 641.
- Ibid., 634; Borges, “Individual Health Care Litigation in Brazil,” 151.
- Wang, “Right to Health Litigation in Brazil,” 625.
- Borges, “Individual Health Care Litigation in Brazil,” 152–53.
- Ibid., 153 (reporting a 1 per cent decrease in state costs from 2014–2015, and a 20 per cent decrease in federal costs between 2014–2015, but suggesting that the latter was the result of drugs being demanded by litigants being more quickly incorporated into the state plan).
- Mæstad, Rakner, and Ferraz, “Assessing the Impact,” 282, table 11.1.
- Everaldo Lamprea and Johnattan Garcia, “Closing the Gap Between Formal and Material Health Care Coverage in Colombia,” Health and Human Rights 18, no. 2 (December 2016): 49–65, 50.
- Yamin, Parra-Vera, and Gianella, “Colombia,” 113; Lamprea, “Judicialization of Health Care,” 440. Colombia’s healthcare system is a public-private hybrid, with private insurance companies and publicly established eligibility criteria, deductibles, premiums, and defined benefits packages. When courts mandate medicines that are not included in the defined benefits package, private insurers are reimbursed for their cost by the government. Yamin, Parra-Vera, and Gianella, “Colombia,” 109–10.
- Lamprea, Forman, and Chapman, “Structural Reform Litigation,” 342. The satisfaction of such judgments took up more than 5 per cent of the health budget in 2009. See Yamin, “Power, Suffering, and Courts,” 353.
- Lamprea, “Judicialization of Health Care,” at 442.
- Yamin, Parra-Vera, and Gianella, “Colombia,” 114–15.
- Lamprea, Foreman, and Chapman, “Structural Reform Litigation,” 342–45; see Decision T-760 of 2008, accessed August 23, 2018, http://www.corteconstitucional.gov.co/relatoria/2008/dT-760-08.htm.
- Ibid.. 347–48.
- Ibid., 350; see also C-313 of 2014, accessed September 8, 2018, http://www.corteconstitudcional.gov.co/relatoria/2014/C-313-14.htm . The Court concluded that while cost-effectiveness requirements were not void in every case, they could not constitutionally be applied in the cases where they contradicted the constitutional jurisprudence, and where dignity is affected.
- Law 1751, enacted on February 16, 2015; see also Lamprea, Foreman, and Chapman, “Structural Reform Litigation,” 347.
- See, for example, Articles 71 and 72 of Law n. 1753, enacted on June 9, 2015. Companies later filed suit asserting that the price control articles violated their own constitutional rights of free enterprise, among others, but their arguments were rejected. I discuss the case, DecisiondC-620–2016, below. For an overview of the development of price controls in Colombia, see Sergio I. Prada et al., “Higher Pharmaceutical Public Expenditure after Direct Price Control: Improved Access or Induced Demand? The Colombian Case,” Cost Effectiveness and Resource Allocation 16, no. 1 (March 2018): 2.
- Prada et al., “Higher Pharmaceutical Public Expenditure,” 6–7.
- Aquiles Ignacio Arrieta-Gómez, “Realizing the Fundamental Right to Health through Litigation: The Colombian Case,” Health and Human Rights 20, no. 1 (June 2018): 139.
- Mæstad, Rakner, and Ferraz, “Assessing the Impact,” 282, table 11.1 (reporting an estimated five hundred cases per year in Costa Rica, and more than a one thousand cases per year in Argentina); Pizzarossa, Perehudoff, and Forte, “Uruguayan Judiciary,” 96, fig. 1 (showing a smaller number of cases in Uruguay, reaching a maximum of forty-two in 2015).
- Paola Bergallo, “Argentina: Courts and the Right to Health: Achieving Fairness despite `Routinization’ in Individual Coverage Cases,” in Litigating Health Rights, 52, 56, 59; Bruce M. Wilson, “Costa Rica: Health Rights Litigation: Causes and Consequences,” in Litigating Health Rights, 140–41, 144; Pizzarossa, Perehudoff, and Forte, “Uruguayan Judiciary,” 97–98.
- It took 1 per cent of the national medicines budget of Costa Rica to provide medicines to just twenty-nine patients who were awarded expensive drugs by courts for diseases including cancer. Wilson, Costa Rica, 146.
- Kapczynski and Berger, “Story of the TAC Case,” 17. The case targeted a cheap and highly effective medicine, and was not followed by individualized claims to medicines, so has not triggered similar criticisms.
- Ahmed v. Union of India, W.P.(C) 7279/2013, slip op. para. 69 (Del. Apr. 17, 2014). The same drug was also awarded by a court in Costa Rica, at a cost of about $175,000 per year. See Wilson, “Costa Rica,” 146.
- Ahmed v. Union of India, para. 1.
- Ibid., para 69.
- One exception is provided by an excellent new paper that argues that courts should assess the adequacy of the state’s attempts to spend efficiently and lower prices, including by using TRIPS flexibilities, when they are faced with plaintiffs seeking access to high-cost medicines that the state argues are not cost-effective. See Pizzarossa, Perehudoff, and Forte, “Uruguayan Judiciary,” 101.
- Ferraz, “Brazil: Health Inequalities,” 82; see also Lamprea, “Judicialization of Health Care,” 441–42 (providing references showing that most of the costs of judicialization at the federal level stem from “expensive biotech drugs for chronic medical conditions like cancer, arthritis, and rare diseases”).
- Wang, “Right to Health Litigation in Brazil,” 627.
- Lamprea, “Judicialization of Health Care,” 442.
- Aaron S. Kesselheim, Jerry Avorn, and Ameet Sarpatwari, “The High Cost of Prescription Drugs in the United States: Origins and Prospects for Reform,” Journal of the American Medical Association 316, no. 8 (August 2016): 858–71, 860, 861 (noting that “brand-name drugs comprise only 10% of all dispensed prescriptions in the United States, [but] they account for 72% of drug spending,” and noting that “the most important factor that allows manufacturers to set high drug prices for brand-name drugs is market exclusivity”). See also the PEW Charitable Trusts, Fact Sheet: Specialty Drugs and Health Care Costs (November 2015), accessed August 23, 2018, https://perma.cc/Z2EU-LFDB
- See Andrew Hill and Graham Cooke, “Hepatitis C Can Be Cured Globally, but at What Cost?,” Science, July 11, 2014.
- “Untangling the Web of Antiretroviral Price Reductions,” Médecins Sans Frontières 2, 18th ed. (2016), accessed August 24, 2018, https://msfaccess.org/sites/default/files/HIV–report–dUntangling-the-web-18thed–ENG–2016.pdf
- Hoffman and Bentes, “Accountability for Social and Economic Rights,” 132.
- Chaves, Vieira, and Reis, “Access to Medicines and Intellectual Property,” 177.
- Ibid., 178 (noting that they were available for one-third of the patented price).
- Lynne Taylor, “Brazilian Judge Annuls Abbott’s Kaletra Patent,” PharmaTimes, March 23, 2012, accessed August 24, 2018, http://www.pharmatimes.com/article/12-03-23/Brazilian–djudge–annuls–Abbott–s–Kaletra–patent.aspx
- Ibid.
- For two superb histories, see Drahos and Braithwaite, Information Feudalism and Sell, Public Power, Private Law.
- “Least developing countries” have a longer timeframe to adhere to this requirement of TRIPS, and there are efforts to extend their deadline indefinitely, for as long they are in the category of least-developing countries. See Agreement on Trade-Related Aspects of Intellectual Property Rights, art. 66, April 15, 1994, Marrakesh Agreement Establishing the World Trade Organization, Annex 1C, 1869 U.N.T.S. 299 (1994) (hereafter TRIPS). Many such countries have patents on medicines already, though, because of the legal legacy of colonialism as well as more recent trade pressures.
- Jagdish Bhagwati, for example, has written scathingly of the inclusion of TRIPS in the WTO. See Jagdish Bhagwati, “Afterword: The Question of Linkage,” American Journal of International Law 96, no. 1 (January 2002): 126, 127.
- Global public goods arguments could be mobilized, after all, to support the use of the global trade regime to produce many other things—why not leverage trade sanctions, for example, to hold governments to account for environmental degradation? That idea is disturbing to many defenders of free trade. See, for example, Bhagwati, “Afterward,” 128, on this point.
- For a history of this period by a leading activist in the movement, see Gaëlle Krikorian, “Free-Trade Agreements and Neoliberalism: How to Derail the Political Rationales that Impose Strong Intellectual Property Protection,” in Access to Knowledge in the Age of Intellectual Property, ed. Gaëlle Krikorian & Amy Kapczynski (New York: Zone Books, 2008), 293–328.
- TRIPS, Article 31.
- Ellen F. M. `t Hoen, On the Global Politics of Pharmaceutical Monopoly Power: Drug Patents, Access, Innovation and the Application of the WTO Doha Declaration on TRIPS and Public Health (Dieman: AMB, 2009), accessed August 23, 2018, http://www.msfaccess.org/content/globald-politics-pharmaceutical-monopoly-power
- One hundred sixty-four countries are members of the WTO today. And following TRIPS, many more agreements have ratcheted IP requirements up further, mostly in bilateral and regional “free trade” agreements. See Susan K. Sell, “TRIPS-Plus Free Trade Agreements and Access to Medicines,” Liverpool Law Review 28, no. 1 (April 2007): 41–75. For a detailed account of how far countries can go with flexibilities in the medicines domain, and the difficulty of implementing them locally, see Amy Kapczynski, “Harmonization and Its Discontents: A Case Study of TRIPS Implementation in India’s Pharmaceutical Sector,” California Law Review 97 (2009): 1571–650.
- See Commission on Intellectual Property Rights, Innovation, and Public Health (CIPR), Public Health: Innovation and Intellectual Property Rights (2006); World Health Organization Consultative Expert Working Group, Research and Development: Financing and Coordination, Research and Development to Meet Health Needs in Developing Countries: Strengthening Global Financing and Coordination (2012).
- CIPR, Public Health: Innovation and Intellectual Property Rights, 15, table 1.4.
- European Federation of Pharmaceutical Associations, The Pharmaceutical Industry in Figures, Key Data 2017 (2017), 14, accessed September 14, 2018, https://www.efpia.eu/media/219735/efpia-pharmafigures2017–statisticbroch–v04-final.pdf
- Association of the British Pharmaceutical Industry, Shares of the Global Pharmaceutical Markets, accessed September 4, 2018, https://www.abpi.org.uk/what-we-do/developing-researchingd-medicines/global-health-and-the-role-of-biopharma/shares-of-the-global-pharmaceutical-markets/
- “Transcript of Bayer CEO Marjin Dekkers Quote at the December 3, 2013 FT Event, Regarding India Compulsory License of Nexavar,” Knowledge Ecology International, February 2014, accessed September 4, 2018, https://www.keionline.org/22414
- “Experts: Ebola Vaccine at Least 50 White People Away,” Onion, July 30, 2014, accessed August 24, 2018, http://www.theonion.com/articles/experts-ebola-vaccine-at-least-50-white-peopled-awa,36580/
- James Suroweicki, “Ebolanomics,” New Yorker, August 25, 2014, accessed August 25, 2018, http://www.newyorker.com/magazine/2014/08/25/ebolanomics
- See, for example, Anthony S. Fauci and Francis S. Collins, “NIH Ebola Update: Working Toward Treatments and Vaccines,” U.S. Department of Health and Human Services, October 14, 2014, accessed August 24, 2018, http://directorsblog.nih.gov/2014/10/14/nih-ebolad-update-working-toward-treatments-and-vaccines/
- Public-sector-based research, particularly R&D sponsored by the military, has been an important source of drugs for diseases that have primary incidence in low- and middle-income countries. See, for example, Donald G. McNeil Jr., “Herbal Drug Widely Embraced in Treating Resistant Malaria,” New York Times, May 10, 2004, accessed August 25, 2018, https://wwwd.nytimes.com/2004/05/10/world/herbal-drug-widely-embraced-in-treating-resistant-malaria.html (discussing artemisinin, a treatment for malaria first isolated by Chinese military researchers as well as mefloquine, an antimalarial drug developed at the Walter Reed Army Institute of Research in the 1960s).
- Harold Demsetz, “Information and Efficiency, Another Viewpoint,” Journal of Law and Economics 12, no. 1 (April 1969): 1–22; see also Amy Kapczynski, “The Cost of Price: Why and How to Get Beyond Intellectual Property Internalism,” UCLA Law Review 59 (2012): 970–1026.
- See, for example, Jennifer Prah Ruger, Health and Social Justice (Oxford: Oxford University Press 2012); Sridhar Venkatapuram, Health Justice: An Argument from the Capabilities Approach (Cambridge: Polity Press, 2011).
- See, for example, Patrice Trouiller et al., “Drug Development for Neglected Diseases: A Deficient Market and a Public-Health Policy Failure,” Lancet 359, no. 9324 (2002): 2188–94 (showing that “of 1393 new chemical entities marketed between 1975 and 1999, only 16 were for tropical diseases and tuberculosis”).
- See Sean Flynn, Aiden Hollis, and Mike Palmedo, “An Economic Justification for Open Access to Essential Medicine Patents in Developing Countries,” Journal of Law, Medicine and Ethics 37, no. 2 (Summer 2009): 184–208.
- Ibid.
- Tribunal Constitutional [T.C.] [Constitutional Court], September 26, 2001, Rol de la Causa No. 01–009007-CO, Salazar Navarro v. Caja Costarricense de Seguro Social (Costa Rica).
- They achieved just one compulsory license, on effavirenz. See Chaves, Vieira, and Reis, “Access to Medicines and Intellectual Property,” 171. That license did, however, reduce the cost of the product by two-thirds.
- Ibid., 177–78.
- Ibid., 175.
- See Ibid., 178.
- Ibid., 178–79.
- Ibid., 181.
- Ibid.
- See MSF Access Campaign, Are Brazilian Pipeline Patents Constitutional?, accessed August 24, 2018, https://www.msfaccess.org/content/are-brazilian-pipeline-patents-constitutional; Carolinne Thays Scopel and Gabriela Costa Chaves, “Initiatives to Challenge Patent Barriers and Their Relationship with the Price of Medicines Procured by the Brazilian Unified National Health System,” Cadernos de Saúde Pública 32, no. 11 (November 2016): 6–7, accessed August 24, 2018, https://doi.org/10.1590/0102-311×00113815. It is not uncommon for constitutional cases to pend for many years before the Constitutional Court, and justices may request additional time to reassess cases and suspend ongoing deliberations. Diana Kapiszewski, High Courts and Economic Governance in Argentina and Brazil (Cambridge: Cambridge University Press, 2012), 105. In 2012, Cristália, a Brazilian pharmaceutical company successfully raised this same argument in a patent dispute before a lower court in Rio de Janeiro. See Taylor, “Brazilian Judge Annuls.” The legal dispute surrounding Abbott’s patent is apparently ongoing, but Cristália has signed an agreement with the Brazilian Ministry of Health to manufacture and distribute the challenged drug. Notably, Cristália is one of the few large locally owned pharmaceuticals in Brazil. See Matthew Flynn, Pharmaceutical Autonomy and Public Health in Latin America: State, Society, and Industry in Brazil’s AIDS Program (New York: Routledge, 2014), 176–77.
- Francisco Rossi, “Civil Society Participation and the Compulsory License Request for Lopinavir-Ritonovir (Kaletra –Abbott),” in Intellectual Property Rights and Access to ARV Medicines: Civil Society Resistance in the Global South, ed. Veriano Terto Júnior, Maria Cristina Pimenta, and AssociaÀ’Àão Brasileira Interdisciplinar de AIDS (Rio de Janeiro, Brazil: ABIA, 2009), 65.
- Ibid., 64–65.
- Ibid.
- Ibid. Patents, they argued, also led to “disease mongering,” because high prices generated incentives to promote higher priced medicines. Ibid., 67.
- Ibid., 66, 68. See also “Colombia’s CL Campaign Story,” Public Citizen, accessed September 14, 2018, https://www.citizen.org/article/colombias-compulsory-licensing-campaign; “Civil society competition request letters and responses,” Public Citizen, accessed September 14, 2018, https://www.citizen.org/article/communications-between-colombian-health-groups-andd-government
- Rossi, “Civil Society Participation,” 81, 69–70.
- Ibid., 71.
- Ibid., 59.
- Luz Marina Umbasia, IFARMA, “Colombian Ministry of Health and Social Protection Violated Health Rights,” accessed September 14, 2018, https://www.citizen.org/english-translationd-colombian-civil-society-statement-supreme-administrative-courts-decision-0
- Ibid.
- Ibid.
- Ibid.
- “Colombian Appeals Court: Ministry of Health Violated Health Rights,” Public Citizen, accessed September 14, 2018, https://www.citizen.org/colombian-appeals-court-ministry-healthd-violated-health-rights
- Decision C-620–2016, accessed August 24, 2018, http://www.corteconstitucional.gov.co/relatoria/2016/C-620-16.htm
- Ibid.
- For more on these cases, and the others described here, see the recent Global Health Justice Partnership report, Hannah Brennan et al., “A Human Rights Approach to Intellectual Property and Access to Medicines,” Global Health Justice Partnership, 2013, accessed August 24, 2018, http://www.yaleghjp.org/human-rights-ip-law—a2m (hereafter GHJP Report).
- F. Hoffmann-LA Roche AG v. Cipla Ltd., I.A. 642/2008 IN CS (OS) 89/2008 (2008) (India), accessed August 24, 2018, https://indiankanoon.org/doc/131401110/
- Ibid.
- Asero Ochieng v. Attorney General, Petition No. 409 of 2009 (Kenya, High Court of Kenya at Nairobi, 2012) at 28–29 para. 73, accessed August 25, 2018, https://ipkenya.filesd.wordpress.com/2012/04/aca-petition-no-409-of-2009.pdf
- Ibid. para. 66.
- Ibid. at para 83.
- Ibid. para 86. Petitioners challenged the “anti-counterfeiting” law for failing to serve public health ends. They argued that its definition of “counterfeit” was too broad, targeting not only products that were substandard or violated trademarks, but also generic drugs that violated patents, including patents in other countries.
- Brief for TAC at 3, para 6.1, Cipla Medpro v. Aventis Pharma 2012 (139/12).
- Ibid.
- Minister of Health v. New Clicks. (September 30, 2005). CCT 59/2004, para 659 (Sachs, J.).
- Cipla Medpro v Aventis Pharma (139/12) Aventis Pharma SA v Cipla Life Sciences (138/12) [2012] ZASCA 108 (26 July 2012) at para 45. The court did accept that the public interest should be considered before awarding an injunction in a patent case, not as a matter of constitutional law, but as a matter of the judicial standard applied to interim injunctions. Ibid. at para 52.
- See David Singh Grewal, Amy Kapczynski, and Jedediah Purdy, “Law and Political Economy: Toward a Manifesto,” at LPEblog.org, November 6, 2017.
- Robert Lee Hale, Freedom Through Law: Public Control of Private Governing Power. New York: Columbia University Press (1952); Robert Lee Hale, “Coercion and Distribution in a Supposedly Non-Coercive State,” Political Science Quarterly 38, no. 3 (September 1923): 470–94.
- Constitutional Court of Peru (EXP N2945–2003 AA/TC): (“when there is any conflict between fulfilling national objectives related to public health, and the realization of the right [to health] and to life . . . the [WTO’s] Doha Ministerial Declaration has provided that . . . while the protection of intellectual property is important for the development of new medicines, the concern about its effect on prices cannot be ignored; hence, any agreements to protect intellectual property rights will not mean an obstruction to member countries to take the necessary steps to protect public health”); see also GHJP report, 19.
- GHJP Report, 27. The latter, more assertive point came in the context of copyright law, in a report by the Special Rapporteur in the Field of Cultural Rights, “Rep. of the Special Rapporteur in the Field of Cultural Rights, Farida Shaheed: The Right to Enjoy the Benefits of Scientific Progress and Its Applications,” ¶ 59, Human Rights Council, U.N. Doc. A/HRC/20/26, May 14, 2012.
- Special Rapporteur on the Right of Everyone to the Enjoyment of the Highest Attainable Standard of Physical and Mental Health, “Report of the Special Rapporteur on the Right of Everyone to the Enjoyment of the Highest Attainable Standard of Physical and Mental Health,” transmitted by Note of the Secretary-General, U.N. Doc. A/63/263, August 11, 2008, 19–47. The Special Rapporteur’s report, however, was not adopted by the Human Rights Council, and its more ambitious aspects are difficult to square with the new Ruggie approach to corporations and human rights. See GHJP Report, 41.
- Olivier De Schutter, “The Right of Everyone to Enjoy the Benefits of Scientific Progress and the Right to Food: From Conflict to Complementarity,” Human Rights Quarterly 33, no. 2 (May 2011): 304–50.
- Ibid., 349.
- See, for example, Holger Hestermeyer, Human Rights and the WTO: The Case of Patents and Access to Medicines (Oxford: Oxford. University Press, 2007).
- Laurence R. Helfer, “Toward A Human Rights Framework for Intellectual Property,” U.C. Davis Law Review 40 (2007): 973–1020; Peter Yu, “Reconceptualizing Intellectual Property Interests in a Human Rights Framework,” U.C. Davis Law Review 40 (2007): 1041–149.
- See UN Committee on Economic, Social and Cultural Rights, General Comment No. 17, The Right of Everyone to Benefit from the Protection of the Moral and Material Interests Resulting from Any Scientific, Literary or Artistic Production of which He or She is an Author, E/C.12/GC/17, January 12, 2006.
- See Anheuser Busch v. Portugal (Appl. No. 73049/01), confirmed by the Grand Chamber of the ECHR; Laurence R. Helfer, “The New Innovation Frontier? Intellectual Property and the European Court of Human Rights,” Harvard International Law Journal 49, no. 1 (Winter 2008): 1–52.
- On more dialogic approaches, see Roberto Gargarella, “Dialogic Justice in the Enforcement of Social Rights: Some Initial Arguments,” in Litigating Health Rights, 232; Roberto Gargarella, “Theories of Democracy, the Judiciary and Social Rights,” in Courts and Social Transformation in New Democracies: An Institutional Voice for the Poor?, ed. Roberto Gargarella, Pilar Domingo, and Theunis Roux (Farnham, UK: Ashgate, 2006), 13; see also Ahmed v. Union of India, W.P.(C) 7279/2013, slip op. para. 38–43 (Del. Apr. 17, 2014) (comparing India’s failure to provide incentives for the manufacture and distribution of orphan drug with efforts of other countries and concluding that without “changes in the applicable laws,” no “promising orphaned drug[s] will be developed” and the “prohibitive cost” of orphaned drugs will not decrease). For an example of a case that mandates affirmative obligations for the government to produce needed medicines—although not going as far as mandating research—see Viceconte, Mariela Cecilia v. Estado Nacional—Ministerio de Salud y Acción Social, [Cám. Cont .Adm. Fed., Sala V] [Federal Administrative Court of Appeals], 2/6/1998. The court concluded that, to fulfill the right to health, the government was required to complete facilities and infrastructure needed to produce and distribute a vaccine proven to be highly effective against Argentine Hemorrhagic Fever. For a summary, see http://www.globalhealthrights.org/health-topics/viceconte-mariela-cecilia-cd-argentine-ministry-of-health-and-social-welfare/ (accessed August 31, 2018).
- For more on these points, see Amy Kapczynski, “What Comes After `Not Enough’?,” Law and Political Economy blog, June 11, 2018, accessed August 22, 2018, https://lpeblog.org/2018/06/11/what-comes-after-not-enough/

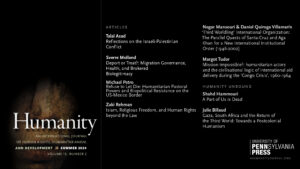
 'Choose Your Bearing: Édouard Glissant, Human Rights and Decolonial Ethics' is now available for pre-order!
'Choose Your Bearing: Édouard Glissant, Human Rights and Decolonial Ethics' is now available for pre-order!  Grab your copy and save 30% OFF using the code NEW30 at checkout :
Grab your copy and save 30% OFF using the code NEW30 at checkout :